Live
- Artemis Coin: The Best Crypto Presale with Explosive Growth Potential
- Rahul Gandhi opposes quota abroad & violates Constitution: BJP MP
- Encounter breaks out in J&K’s Reasi
- RG Kar case: CBI custody of Sandip Ghosh, Abhijit Mondal extended till Sep 25
- J&K: Home Voting begins in all six Kathua Assembly segments
- Gurugram: Biker killed after being hit by SUV
- Bengal doctor’s body bars ex-member from all organisation activities over RG Kar case
- Centre and Seers serious over Tirumala Sacrilege
- LG ELECTRONICS ORGANIZES GRAND TECH SEMINAR IN HYDERABAD
- Tirupati Laddus turns non-vegetarian Pilgrims from Karnataka begin shunning the temple
Just In
Over 41 years up to 2016, a national health programme for children has led to a 68 per cent drop in India\'s infant mortality rate (IMR), but the IMR of 41 deaths per 1,000 live births is still worse off than poorer neighbours like Bangladesh (31) and Nepal (29).
Over 41 years up to 2016, a national health programme for children has led to a 68 per cent drop in India's infant mortality rate (IMR), but the IMR of 41 deaths per 1,000 live births is still worse off than poorer neighbours like Bangladesh (31) and Nepal (29).
It is now 42 years since the integrated child development scheme (ICDS) the world's largest integrated early childhood programme was launched, and its successes and failures mirror the country's inability to improve health services to match the growth in its economy, which grew 21 times or 2,100 per cent between 1975 and 2016.
The scheme, launched on October 2, 1975, was a response to the challenge of providing pre-school and non-formal education and to break the cycle of malnutrition, morbidity, reduced learning capacity and mortality.
ICDS has reached 99.3 million beneficiaries and has 1.4 million anganwadi centres (AWCs) across the country, as of December 2016, the Women and Child Development Ministry told the Lok Sabha in March.
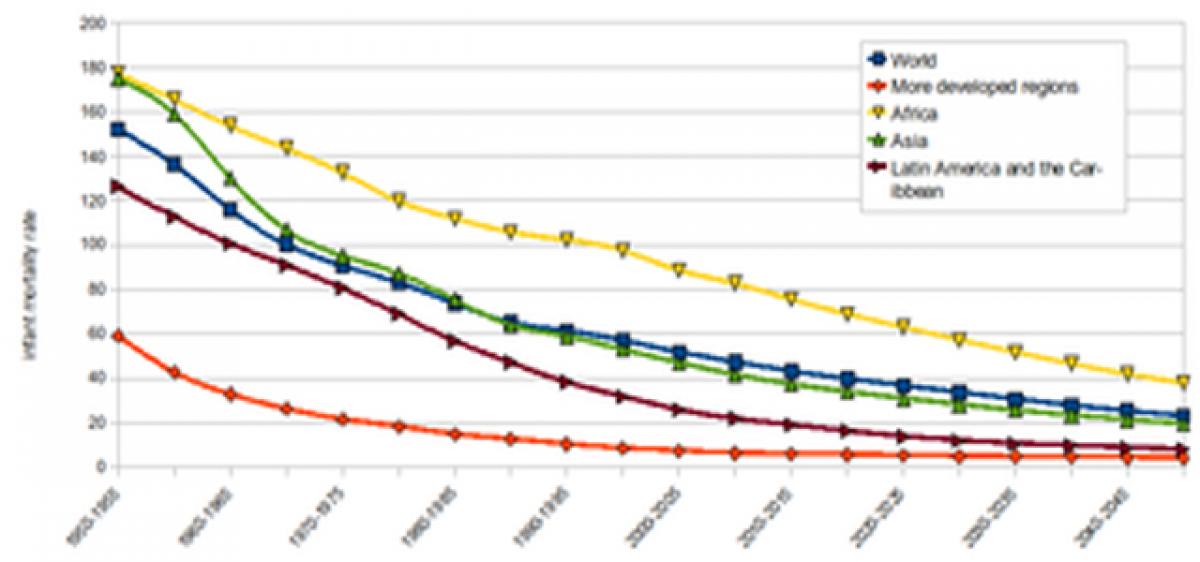
India has reduced its infant mortality rate (IMR, deaths per 1,000 live births) by 68 per cent, as we said, in the last 41 years from 130 in 1975 to 41 in 2015-16, as data from the National Family Health Survey 2015-16 reveal.
Yet, India's IMR of 41 deaths per 1,000 live births is worse off than poorer neighbours Bangladesh (31) and Nepal (29), and the African nation of Rwanda (31). Even its under-five mortality rate of 50 deaths per 1,000 live births is worse than Nepal (36), Bangladesh (38) and Bhutan (33).
There has been a 4.7 per cent increase in the ICDS allocation in Union budget 2017-18 -- from Rs 14,560 crore in 2016-17 to Rs 15,245 in 2017-18. But this was after a bigger reduction in the allocations during 2015-16.
Yet, "...more allocations need to be made both at the Union and state level, considering the severity of malnutrition in India. Also, decreasing the work load of the overburdened anganwadi workers and improving their capacity to support the various services under the programme calls for an enhanced budget allocation," the budget analysis by Centre for Governance and Budget Accountability noted.
The ICDS is aimed at the holistic development of children under six and providing nutritional and health support to pregnant and lactating mothers. There are six services that fall under ICDS: Supplementary nutrition, immunisation, referral services, health check-up, pre-school non formal education, and health and nutrition education.
Three of these immunisation, health check-up and referral services are delivered through the public health system by the Ministry of Health and Family Welfare. The others are delivered through the Women and Child Development Ministry. The idea was to integrate the services together to improve overall impact.
From not actually covering all eligible children to having infrastructural gaps, many deficiencies of the ICDS have been documented by various reports over the years. Around 50 per cent of the total eligible children were found to be enrolled at anganwadi centres and the effective coverage as per norms is only 41 per cent of those registered for the ICDS benefits, according to this 2011 evaluation of ICDS by the erstwhile Planning Commission across 100 districts in 35 states.
"Anganwadi workers are overburdened, underpaid and mostly unskilled, which affects the implementation of the scheme," the report noted. Sixty percent of the AWCs did not have their own building, and 25 per cent were functioning in semi-pucca/kuccha buildings or partially open space, a 2012 audit on ICDS by the comptroller and auditor general (CAG) of India the government's auditor found.
Fifty two percent of AWCs did not have a toilet and 32 per cent did not have drinking water facilities -- which led to sanitation and hygiene problems the CAG's report noted. Besides the infrastructure issues, the auditors found 33 to 47 per cent of children were not weighed from 2006 to 2011, and the data on nutritional status of children had discrepancies.
The auditors found that the funds were not released for critical aspects of the scheme and a large portion of the funds released were for salaries; they also noted that "the follow-up action on the internal monitoring and evaluation by the ministry was not adequate".
Nearly 60 percent of AWCs were still awaiting their flexi funds of Rs 1,000 per annum for meeting emergency costs such as referral arrangements, shortage of medicines and utensils, a 2016 survey across 300 AWCs, spread across 10 districts in five states, by Accountability Initiative, a public research initiative at Centre for Policy Research, Delhi, found.
Fourteen percent AWCs reported a shortage of grains and 41 per cent reported a delay in getting grains or money to buy grains the survey found. (In arrangement with IndiaSpend.org)
By Swagata Yadavar

© 2024 Hyderabad Media House Limited/The Hans India. All rights reserved. Powered by hocalwire.com







