Black Fungus A battle within the war
Black Fungus A battle within the war
Dr Tarjani Vivek Dave, Senior Ophthalmologist – Oculoplasty Specialist, L V Prasad Eye Institute says that Mucormycosis called Black Fungus can occur either concurrent to the Covid-19 infection or in the early post-recovery phase. Patients with pre-existing, poorly controlled diabetes are more at risk for Mucormycosis.
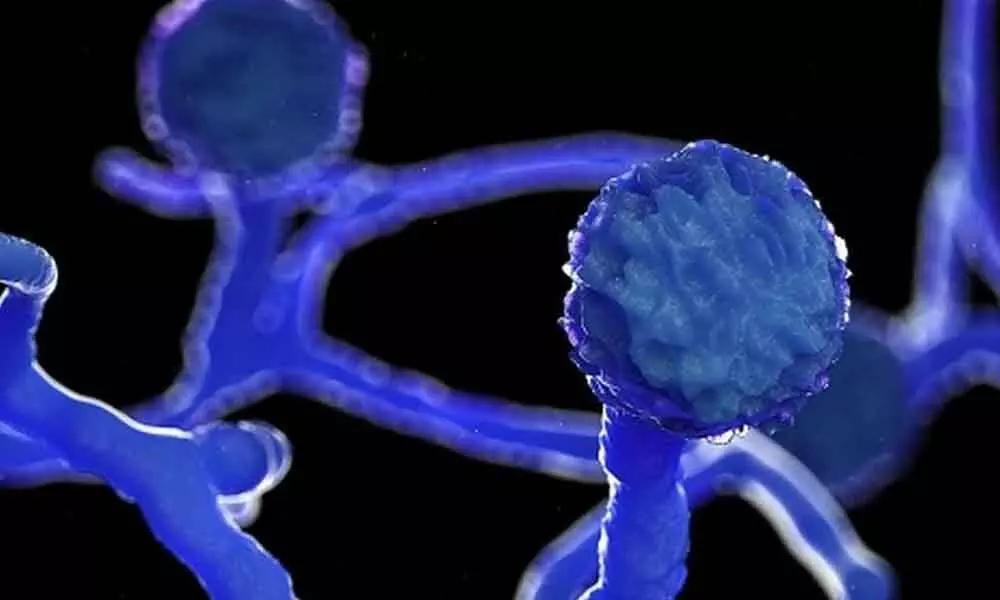
They should be vigilant as the second wave of Covid-19 that India is witnessing is far more severe with an increase in the incidence of an unusual fungal infection. Popularly known as Black Fungus, its scientific name is Mucormycosis. It is caused by a ubiquitous fungus found all around us in soil, water and air called Mucor.
Q.What's causing this sudden spike in Mucormycosis in Covid-19?
Black Fungus or Mucormycosis can occur either concurrent to the Covid-19 infection or in the early post-recovery phase and affect the sinuses, eyes and brain. Even though Mucor is present in the oral and respiratory lining of healthy individuals, it does not manifest as an infection in the presence of a healthy and intact immune system. Generally, this infection occurs in patients with uncontrolled diabetes, undergoing cancer chemotherapy, on long-term steroid therapy, following organ transplantation, extensive burns and poly-trauma (severe injuries).
Q.How Covid-19 causing the Black Fungus?
The Covid-19 virus causes a reduction in the lymphocyte (white blood cell) levels in the body. WBCs are the body's first line of defence against infections. Its failure allows for Mucor to attack the body and spread in the body tissues. The current Covid management protocols require judicious but high dose steroid usage in those patients whose lungs have got affected. While helping to bring the Covid-related damage under control, the counter-effect of such high dose steroids is suppression of the body's immune mechanisms, which in turn makes our body more vulnerable to the adverse effects of this Black Fungus.
Q.Do the drugs used in treating Covid-19 causes Black Fungus?
Certain drugs called immunomodulators used to treat severe cases of Covid-19 can cause immunosuppression. ICU admissions with long-term oxygen inhalation may result in a drop in oxygen mask hygiene. If the patient has pre-existing, poorly controlled diabetes, then, they are more at risk of developing Mucormycosis.
As the severity of the second wave is far more intense, more patients are being put on steroids and oxygen, and hence the increase in the cases of Black Fungus.
Q.What are the common symptoms?
l Any kind of facial pain
l Pain over the sinuses (cheekbones)
l Stuffy nose
l Blood-stained or black nasal discharge
l Drooping of the upper eyelid
l Unusualbulging of the eyes
l Restricted movement of the eyeball
l Sudden redness and extreme swelling over the eyeball
l Sudden decrease in vision
l Black lesions on the palate or dental pain
If the patient experiences any such symptoms, they should immediately consult a specialized eye surgeon, preferably an Oculoplasty Specialist. Alternatively, an ENT surgeon can also be consulted. Patients can also avail teleconsultation if they are in isolation or under hospital admission.
Q.What is the available treatment?
Mucormycosis is a very invasive infection with significant morbidity and mortality. Blood tests to check sugar levels, nasal swabs and MRI scan are generally done to find out the presence and extent of the Mucor infection.
Early and localized infections can be treated with intravenous and local anti-fungal injections followed by a long course of oral anti-fungal medications. Extensively spread infections require aggressive sinus surgery to clear the internal contents of the cheekbones and injections behind the eye. In a lot of these cases, unfortunately, the entire eyeball may need to be removed to contain the infection and avoid fatality.
Precautions
To reduce the risk of contracting Mucormycosis, the patients can consult their treating physician to ensure good control of blood sugar both during and after recovery from Covid-19. Before your physician puts you on a particular treatment plan, diligently list out to them the physical ailments that you, especially diabetes, high blood pressure, etc. Steroids should be used very judiciously during active Covid-19 infection, i.e. only when the saturation on room air falls below 94, and that too under the care of an expert who can monitor for blood sugar rise and treat promptly. Those under home isolation may not need any steroid treatment. Hygiene of the oxygen masks and humidifiers should be maintained with utmost care. Eat healthy, stay stress-free and follow the Covid precaution protocols. These small tips would hopefully help keep this fungus at bay!

