Live
- YouTube Tests AI-Powered Music Remixes for Creator Shorts
- Hyderabad: Man Dies of Cardiac Arrest While Offering Prayers at Temple
- Suriya’s ‘Kanguva’ Smashes Rs 2.2 Crore in Advance Bookings
- Is There Life on Uranus? New Findings Suggest Its Moons May Hold the Key
- Equipping the next generation
- Today is World Kindness Day: A celebration of compassion and unity
- AI-driven dataset to reveal new insights around diabetes
- Researchers develop new portable knee rehab device to revolutionise post-surgical therapy
- Why Australia's Binar CubeSats Burned Out Early: Solar Activity's Devastating Impact on Satellites
- Tyagaraja’s Legacy Celebrated in Ballet
Just In
ASHA (Accredited Social Health Activist) workers and multi-purpose workers are more focused on maternal and child health targets and other diseases than leprosy,” said Anand.
For three years, Uttar Pradesh farmhand Pradeep Kumar, 24, has been treated for a disease that India largely eliminated 11 years ago: Leprosy, one of humankind’s oldest diseases - it is commonly mentioned in the Bible - is notorious for the visible disfigurement of victims and their subsequent ostracisation.
In 1991, when India began economic liberalisation, leprosy was reported in nearly 26 of 10,000 people. Within 14 years, that prevalence rate – thanks to concerted efforts and multi-drug therapy - had been cut 25 times to less than one per 10,000, the World Health Organization (WHO) threshold for “elimination” as a public-health problem.
Indeed, leprosy appears to have dropped off the government’s radar. Today, Kumar is one of roughly 125,000 Indians who have consistently been diagnosed with leprosy every year, 58 percent of the new cases detected globally. The prevalence rate is about 0.69 per 10,000, but this means 88,833 Indians still have leprosy.
These are the official data. India could have twice as many leprosy cases as reported, even up to four times, said Sunil Anand, executive director of The Leprosy Mission Trust India, an NGO running 14 hospitals. For instance, a 2013 study based in Uttar Pradesh and a 2009 Maharashtra study point to India’s under-reporting of leprosy.
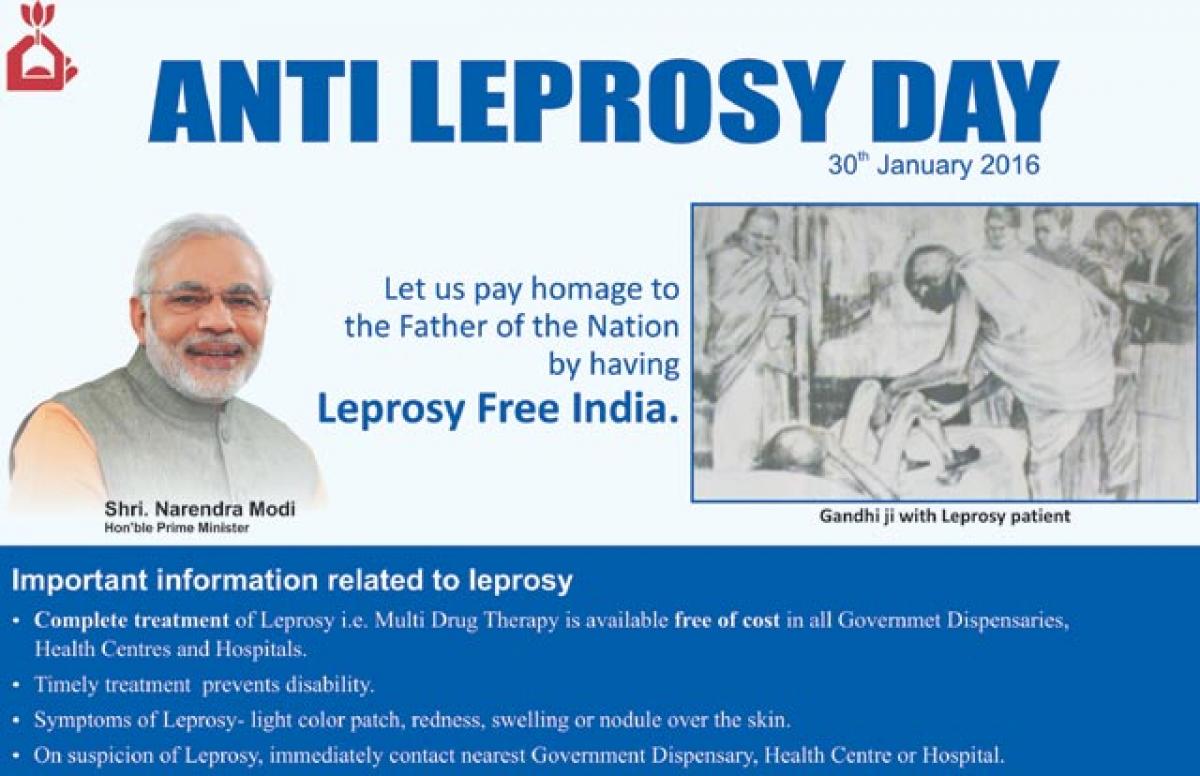
When India’s fight against leprosy stagnates, so does progress towards a leprosy-free world. New global targets hope to restart India’s battle against leprosy Earlier this year, the WHO unveiled a new anti-leprosy strategy, with a 2020 deadline and targets that will compel India to get moving on leprosy again.
Target 1: Reduce the number of children diagnosed with leprosy-affected disabilities to zero. In India, of the 11,365 new child cases identified in 2014, 245 had visible deformities caused by leprosy. In technical parlance, such cases are called grade-II disabilities.
Target 2: Reduce the new patients diagnosed with leprosy-related deformities to less than one per million. India’s grade-II disability rate has risen from 3.72 per million to 4.48 per million over the last three years.
Target 3: Overturning of laws that allow discrimination against leprosy patients.
Reducing the number of new cases with leprosy-related deformities hinges on early detection and treatment, something India is currently not focusing on.
After India eliminated leprosy as a public health problem in December 2005, leprosy services fell off the government’s priority list. They were integrated with general health services to cut costs. Identifying leprosy was now the responsibility of poorly trained frontline primary health care workers, who also run higher priority programmes.
“ASHA (Accredited Social Health Activist) workers and multi-purpose workers are more focused on maternal and child health targets and other diseases than leprosy,” said Anand. “Also, they are trained only to suspect and refer (to doctors) possible leprosy cases.”
A lot of patients delay treatment because of the continuing stigma of leprosy. Today, however, “we are relying too heavily on self-reporting by patients, which presupposes high awareness and an encouraging social environment, while frankly, we are not very good at either,” said Bhushan Kumar, former head, Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education & Research, Chandigarh.
Instead, Bhushan Kumar suggested surveillance in endemic areas to identify (and treat) hidden cases, and vaccinating or prescribing preventative medicine to people at high risk of contracting leprosy, such as those with a relative suffering from the disease and those living in endemic areas, such as Chhattisgarh and Dadra & Nagar Haveli, which have not achieved “elimination”.
“Research shows that a second dose of BCG (tuberculosis vaccination) or the Mycobacterium W (MIP) vaccine could help prevent the development of leprosy in a large number of patients,” he said.
Charu Bahri
(In arrangement with IndiaSpend.org)

© 2024 Hyderabad Media House Limited/The Hans India. All rights reserved. Powered by hocalwire.com







